Services We Provide
Appointment Scheduling
Unified scheduling
Efficient rescheduling
Canceling to reduce no-show rates


Eligibility & Verification
Insurance eligibility verification is the first and one of the key steps in medical billing and coding process. Most of the medical claims are denied or delayed by the insurance companies mainly due to incorrect or inadequate coverage details provided by the patients during their visits or when the current coverage information is not updated by the hospital or administrative staff. This directly impacts the cash flow of the company by delaying the reimbursements.
Authorization & Referrals Check
Provide notification phone calls
Online forms approval
Follow-ups

Patient Collections(Inbound & Outbound)
Outbound marketing—also called “push marketing” or “interruption marketing”—is when a marketer contacts prospects, hoping for engagement.
Inbound marketing—also called “pull advertising”—helps customers find you, rather than you seeking them out. Marketers using inbound methods don’t interrupt a prospect’s flow. Rather, they prioritize placing compelling content where prospects are likely to find it organically.
Demo Entry/Charge entry
We follow a structured charge entry process and check all the cost-related data for accuracy and legitimacy to prevent denial of the claims submitted

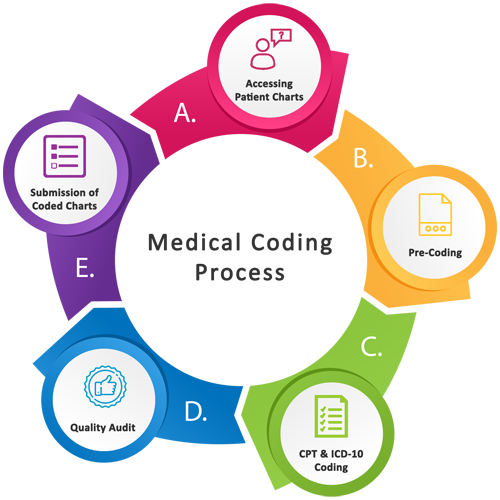
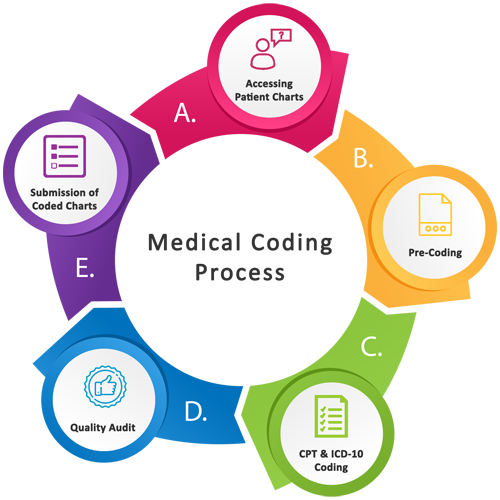
Medical Coding
Insurance processing demands a quick and efficient submission of patient information from healthcare organizations. The efficiency in submission determines the rate of approvals and the denials of claims. In such a case, there is an immense need to make the insurance claims filing process highly accurate and fast. Medical coding involves assigning codes and categorizing patient records which makes the medical practice management process proficient. Each patient chart is assigned a particular code that helps in the easy access of medical information for insurance purposes.
Pharmacy Billing
When you outsource your medical coding services to HealthTeq, you will not only optimize your revenue while reducing compliance risks, but also increase your cash flow by reducing lag days, improving claim submissions, and lessening the burden of administrative expenses.
Our comprehensive coding services are available as part of our full medical billing services or as a standalone service for organizations doing their own billing.

Pharmacy Billing Softwere
Are you struggling to survive in an economy where margins keep reducing and the competition keeps increasing? Are you looking for a system which can automate your billing management systems? Then, pharmacy billing is what you need! Irrespective of the sector and the vertical, companies are relying on automating their management systems.
Laboratory Billing
Running a busy medical lab will definitely keep you on your toes. As compared to a physician’s office, urgent care facility, or other place of healing, you likely will be seeing many more patients coming through your doors every day. These patients will arrive to fulfill their doctor’s orders for tests or because they are being screened for using illicit substances.

Electronic claim submission
The modern healthcare world started shifting towards electronic claim submission for timely claim payments. So if you haven’t switched over to electronic claim submission, may cause your practice to decline in value and effectiveness. You may be thinking about how to speed up your claim process. The easy way is to go with the best medical billing software that includes provisions for electronic claims submission. Here is how electronic claim submission speeds up your claim process and results with more timely payments.
Payment posting
In the overall process of medical revenue cycle management (RCM), payment posting is often relegated to the “when I get around to it” list—meaning it often gets left undone. At first it may seem like an administrative detail that isn’t very important since you’ve already received payment, but that’s a short-sighted view of what is actually a very important part of medical billing, if you want to maximize revenue.

Denial posting
Denial tracking and payment posting are time consuming yet fundamental features of the revenue cycle management (RCM). Successful implementation of these processes can have a major impact on efficiency, patient satisfaction and financial performance of your medical practice.
AR Follow up
Account receivable (also known as A/R) is a term used to denote cash owed by organizations for practices and services rendered and billed. Any payments from payers, patients, and other guarantors are measured as A/R. A goal of every organization is to make sure that it gets’ paid correctly and in a timely manner. An upsurge in A/R from a one period of time to another is a clear indication that amounts are not getting collected upfront, as they should be. This can result in cash flow complications in case it is not corrected.


Denial Management follow up
Healtheq offers a full suite of healthcare denial management services that include A/R follow-ups, claim status checks, resolution of denied claims, preparing appeal letters, etc. – all done with one goal in mind, which is to collect revenue due for medical billing services rendered.
It is important to note that terms, claim denial and claim rejection, are often used interchangeably by office billing personnel as both may be considered a part of the denial management process. Rejected claims will not be processed as they have not been received/accepted by the payer. Therefore, these claims do not make it into the adjudication system.
Appeals/Follow up on appeals
Always keep a copy of the appeal on file for your reference. Appeal work does not end with a successful submission. Once you have allowed enough time for the documents to be received and reviewed, you will need to begin the follow-up process.


Provider credentialing
PECOS & CAQH Enrolment
Provider Credentialing and Contracting with Federal, Commercial and IPA payers
Report generation for provider business
The report generation tool is a powerful feature for building template-based documents for all of your opportunities. Use this tool to create report templates, then automatically fill them with the proper content for any opportunity in your company pipeline to create custom reports with the minimum amount of time and effort. You no longer need to look for the data each time you create a report for a new opportunity, because C2P is pulling all the relevant information into the reports in the right place for you.


Workers' Compensation Billing
Workers’ compensation, also known as workers’ comp, is a type of health insurance that covers injuries incurred at work. Employers must purchase workers’ comp directly in most states, although some states administer these policies. Workers’ compensation billing service providers must be aware of the guidelines for their particular state, including requirements and limitations.
Auto Insurance Claims
even from the scene of the accident—regardless of who is at fault. Even if the accident appears minor, it’s important to let your insurance company know about the incident and to find out whether your auto insurance policy covers you for the particular loss.


No Fault A/R follow-up
Medical billing Account receivable (AR follow-ups) and the revenue cycle management handled by an in-house workforce is a thing of the past. In this expertise driven era, everything is outsourced to authorities of their respective fields. Account receivable follow up & management is one of the chief driving forces pertaining to the cash flow. A strategy in place for AR follow up and management ensures physicians attain their business goals.
Hospital Billing
Spending time in the hospital is very expensive. Rather than giving you an itemized list of everything that might go into a hospital stay, I’ll talk about something that should be almost as good: bills from a hospital, complete with final payments. That should give us a pretty good idea of the value of hospital services, since insurance companies have access to all the costs and specialize in being able to offer the minimum amount any institution is likely to accept.


Physician Billing
Do you know that medical billing errors can complicate the relationship between patients and insurers as it eats away more time and money rectifying errors while causing inconvenience to everyone involved? Without diligently billing patients and collecting payments in time, you could be operating at a loss. Don’t let that happen to you.
If you dread getting bills out to file claims, you are not alone. Inefficient billing habits can get you tied up with claims rejection and a chain of activities to tidy the mess. If this is you, outsourcing physician billing process is the way to go. Working side by side with an experienced physician billing services company like Flatworld Solutions can prevent billing concerns from coming in the way of patient care and services.
Software we Use